Coxarthrosis of the hip joint is a degenerative-dystrophic process that occurs in the articular joints of the femoral head and the pelvic acetabulum. The disease is more typical for middle-aged people and the elderly, although it can also occur in young people, including children. Often, its development is preceded by injury, as well as some pathologies of an inflammatory and non-inflammatory nature, and pain and stiffness of movement become the main signs of degenerative-dystrophic processes in the hip joint. In its development, the disease goes through several stages, and if in the early stages it can be treated conservatively, then in the latter stage, the treatment of coxarthrosis of the hip joint is effective only with surgery. Otherwise, the pathology will lead to severe disorders or even complete immobilization.
What is coxarthrosis of the hip joint and the mechanism of its development
Coxarthrosis, also called osteoarthritis and deformed arthrosis, is a complex disease of the hip joint (HJ), accompanied by progressive cartilage destruction. Over time, this leads to deformation of adjacent bone surfaces, as well as the formation of bone growths on them, called osteophytes.
According to statistics, coxarthrosis accounts for about 12% of all diseases of the musculoskeletal system. In terms of frequency of occurrence, it is the second after gonarthrosis of the knee joint, but the risk of getting a deformity with it is much higher.
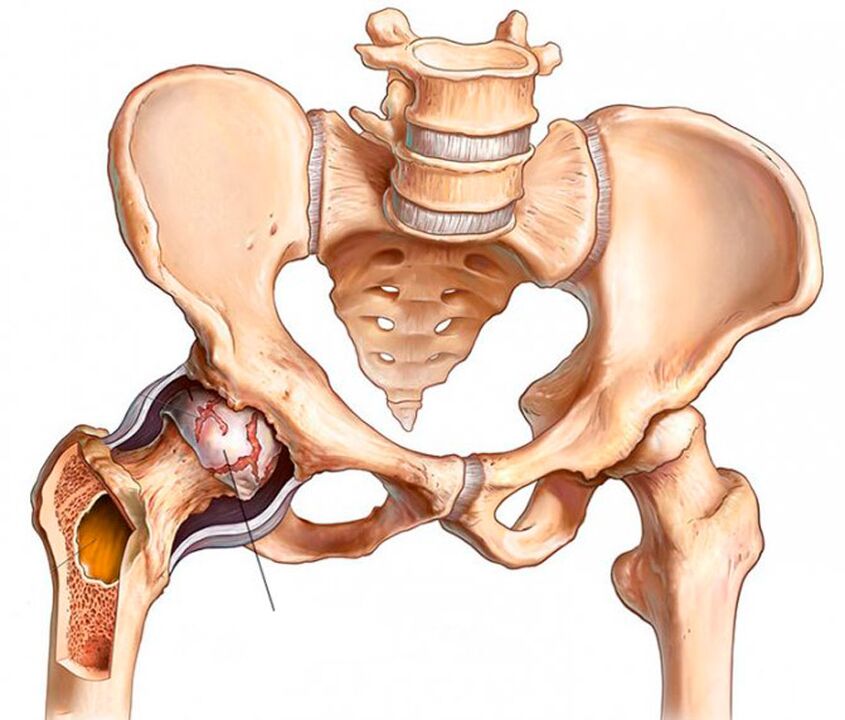
The two hip joints are the largest joints in the body. Each of them is formed by the femoral bone and the pelvic acetabulum. The femoral head is located in a cup -shaped niche of the pelvic bone and moves freely in different directions. The structure of this joint makes it possible to flex and bend, add and abduct, and also rotate the thigh.
To prevent movement from causing discomfort, the surfaces of the bones in contact with each other are covered with an elastic layer called hyaline cartilage. He is the one who allows the femoral head to slide easily in the acetabulum. Also, hyaline cartilage provides stabilization and cushioning of the hip joint during movement.
The entire joint is immersed in a type of case called an articular capsule. It contains a synovial membrane that synthesizes synovial fluid. He is the one who lubricates the surface of the cartilage, ensuring the flow of water and nutrients into it, that is, responsible for maintaining the normal structure of the cartilage tissue.
Above the joint capsule is a group of femoral and pelvic muscles, with the help of which the joint moves. The hip joint is also surrounded by a group of ligaments that ensure the stability of its position within physiological boundaries.
Because the hip joint is subjected to heavy loads on a daily basis, it is prone to rapid wear and injury. The risk of such a change significantly increases the impact of several unfavorable factors that are almost inevitable in the modern world, but it will be discussed below. This explains the high prevalence of coxarthrosis.
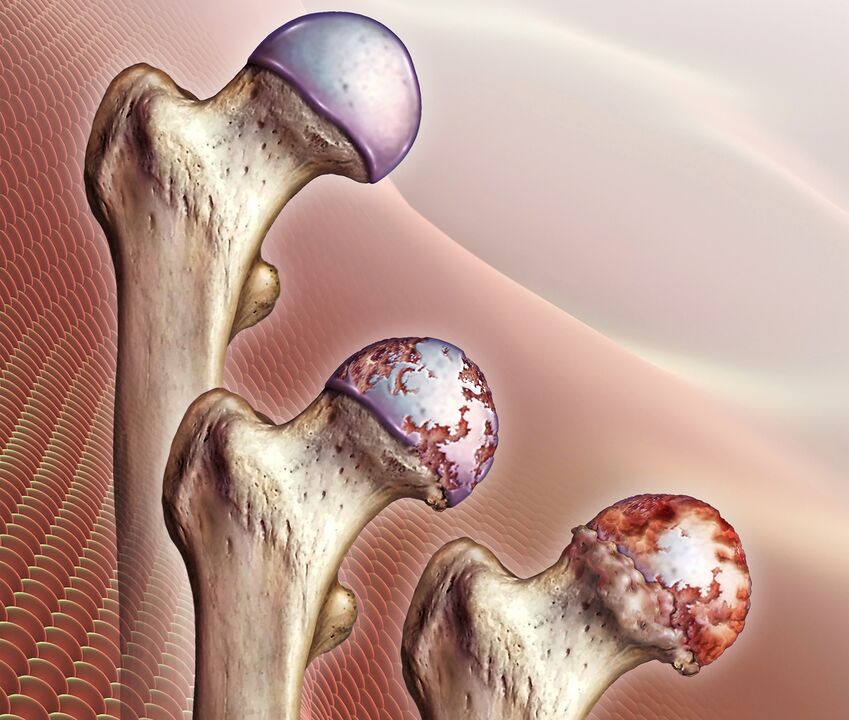
As a result of the influence of negative factors, there is a violation of the production of synovial fluid. Gradually, its quantity decreases, and its qualitative composition also changes: it becomes viscous, thick and is no longer able to fully nourish the cartilage. This leads to acute nutritional deficiency and progressive dehydration of hyaline cartilage. As a result of such changes, the strength and elasticity of cartilage tissue decreases, it peels, cracks and decreases in volume. All this prevents the smooth sliding of the femoral head in the pelvic acetabulum, which leads to the appearance of signs of hip coxarthrosis.
Gradually, the interarticular gap narrows, increased friction occurs between the surfaces of the articular bone, and bone pressure on the hyaline cartilage increases. This leads to greater injury and wear, which inevitably affects the biomechanics of the hip joint and a person’s well -being.
Hip joint failure has a negative impact not only on the biomechanics of the lower leg, but also the overall locomotor apparatus. This often results in disability.
As pathological changes develop, the hyaline layer gradually disappears completely, leading to bone surface exposure and a critical increase in load on the bone joints. During movement, the femoral head is no longer covered by anything and rubs directly against the surface of the pelvic acetabulum. Besides the fact that it completely limits mobility and causes unbearable pain, the bones press against each other, at the same time.
When the articular bone changes shape, bone growths (osteophytes) form on its surface. They can have sharp edges and injure the muscles around them. This triggers severe pain in the groin, legs and buttocks. Therefore, the patient unconsciously tries to save the affected hip joint and avoid movement in it. Lack of adequate load on the muscles leads to gradual atrophy, which exacerbates mobility problems. This results in lameness.
Reasons for development
Coxarthrosis of the hip joint can be primary or secondary. In the first case, the causes of its development cannot be found, that is, the disease develops on its own for no apparent reason. Secondary coxarthrosis is the result of several changes in the state of the musculoskeletal system or lifestyle characteristics, in particular:
- hip joint injuries, including fractures, dislocations, bruises, sprains or ruptures of surrounding ligaments, chronic micro damage, etc. ;
- exhausting physical work;
- sedentary lifestyle;
- obesiti;
- chronic infectious processes in the body;
- rheumatoid arthritis, gout, tendonitis, bursitis;
- endocrine diseases, metabolic and hormonal disorders, including diabetes mellitus;
- congenital malformations of the hip joint (dislocation, dysplasia);
- aseptic necrosis of the femoral head;
- spinal pathology of various types;
- genetic predisposition;
- smoking addiction.
In most cases, the development of coxarthrosis of the hip joint is due to inevitable age -related changes, and the presence of other factors from the above circles only increases the risk of its occurrence and increases the rate of development.
Symptoms and degrees
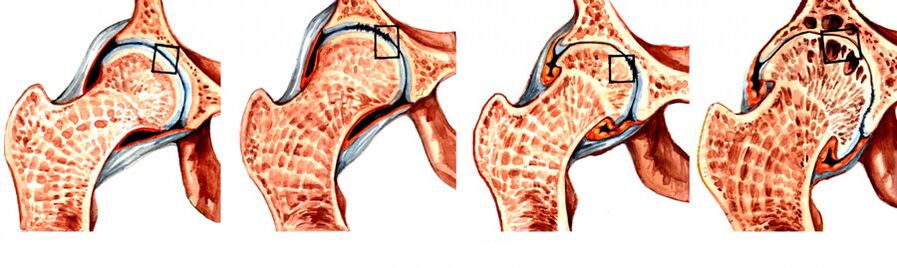
During coxarthrosis, 4 degrees of development are distinguished, of which 1 is the simplest. At first, the disease may be asymptomatic or manifest as mild pain. More often it occurs after vigorous physical exercise, long walks or at the end of a busy day. In the first stages of disease development, discomfort is usually associated with fatigue and is considered the norm. Therefore, very rarely, coxarthrosis of the hip joint is diagnosed in the first stage of development.
Visible signs of coxarthrosis begin to appear in the 2nd stage of its development, when the joint space is narrowed by almost half, and the femoral head is displaced and deformed. With the transition to the 3rd stage, the pain becomes unbearable and can bother a person even at night, they tend to radiate to the hips, hamstrings, groin and buttocks. Since joint space is almost non -existent, and multiple osteophytes form on the bone surface, free movement in such situations is impossible. Therefore, the patient had to use a cane or crutches.
So, the main symptoms of hip joint coxarthrosis are:
- Restriction of mobility - at first, patients may notice the appearance of difficulty in performing rotational movements of the legs, but over time, morning stiffness and swelling of the HJ join them. Because of that, a person needs a few minutes to warm up and, so to speak, take a walk to restore a normal range of motion. Gradually, it becomes increasingly difficult for the patient to perform leg movements.
- Characteristic reflection - occurs when walking, as well as flexion or extension of the hip joint. It is the result of friction of the bone surfaces with each other and with coxarthrosis accompanied by sharp or dull pain.
- Pain syndrome - initially the pain appears after doing physical exercise and somewhat subsides after a long rest. Acute attacks can be provoked by weight lifting or hypothermia, as coxarthrosis is often complicated by the addition of inflammation of the synovial membrane. As the disease progresses, the pain becomes more frequent, lasts longer, and becomes worse.
- Thigh muscle spasm - is the result of pinching of nerves and weakening of the ligament apparatus, so muscle spasm compensates to keep the head of the femur in the acetabulum. Also, muscle spasms can be provoked by the addition of synovitis.
- Lameness - occurs in the last stages of disease development, because the deformation of the bone surface gives rise to the appearance of flexor muscle contractures. Therefore, one cannot fully straighten the leg and maintain it in this position. Also, patients may inadvertently limp to transfer weight to a healthy half of the body, as this helps reduce pain intensity.
- Leg shortening - observed with stage 3 coxarthrosis. The leg on the side of the affected hip joint may be shortened by 1 cm or more as a result of narrowing of the joint space, decreased muscle tone, and a flat femoral head.
In the last stage of development, the femoral head unites with the acetabulum, leading to complete immobilization of the foot and disability.
At the same time, degenerative-dystrophic changes can be observed in one hip joint or both. Accordingly, characteristic symptoms will be observed either on one side or on both at once, but in the latter case, their severity on the left and right may differ.
Diagnostics
Doctors can suspect the presence of coxarthrosis of the hip joint based on patient complaints, external examination and functional test results. Be sure to measure leg length during visual inspection. For this, the patient is asked to stand and straighten his legs as much as possible. Measurements are taken between the anterior axis of the pelvic bone and any structure of the knee, ankle or heel bone. But if both hip joints are simultaneously affected by coxarthrosis, the data obtained will be uninformative.
But because the typical symptoms of coxarthrosis can accompany some other inflammatory and non -inflammatory diseases, instrumental examination methods are mandatory for patients to accurately diagnose the pathology. It can be:
- CT or X -ray of the hip joint - images show destructive changes in it, narrowing of the joint space, osteophyte formation and deformation of the bone surface;
- MRI is the most informative screening method that allows you to accurately assess the nature of changes in cartilage structure, ligaments, and the nature of blood circulation in the hip area.

Patients are also given laboratory tests to assess their general health and detect diseases that can cause coxarthrosis. Ia:
- UAC and OAM;
- blood chemistry;
- rheumatic tests;
- hip joint puncture with biochemical studies.
The task of diagnosis is to distinguish hip coxarthrosis from gonarthrosis (damage to the knee joint), as well as radicular syndrome that occurs with osteochondrosis, as well as protrusion and hernia of the intervertebral disc. Also, the symptoms of coxarthrosis may resemble the manifestations of trochanteric bursitis and the atypical course of ankylosing spondylitis, which requires a full examination to find out the true cause of pain and restriction of movement.
Conservative treatment
Conservative treatment of hip coxarthrosis is effective only in the early stages of the disease. It is selected for each patient individually and may include a variety of different methods, each of which will complement the other. Therefore, as part of the treatment of coxarthrosis of the hip joint, patients can be prescribed:
- drug therapy;
- exercise therapy;
- physiotherapy;
- plasmolifting.
In order for conservative treatment to be effective, patients need to eliminate the effects of several factors that contribute to the development of hip coxarthrosis. If you are overweight, it is very important to reduce it as much as possible. This will reduce the load on the affected joint and the risk of development of degenerative-dystrophic processes.
You should also stop smoking and normalize the mode of physical activity, avoid excessive load, but do not sit all the time. To prevent further destruction of the hip joint, it is recommended to wear special bandages and orthoses. They provide a secure fixation on the joint and support it during movement.
Medical treatment
The therapeutic nature of the drug is chosen strictly individually. In most cases, patients are prescribed:
- NSAIDs-drugs that simultaneously have analgesic and anti-inflammatory effects (available in the form of tablets, injections and topical agents);
- corticosteroids - drugs with strong anti -inflammatory effects, prescribed if NSAIDs do not give a clear effect;
- chondroprotectors - contribute to the activation of the process of regeneration of cartilage tissue, but their effectiveness has not been proven;
- muscle relaxants - drugs that reduce muscle tone and eliminate cramps, which are needed when spasms of muscles or certain groups against the background of severe pain;
- preparations to improve blood circulation - most often used in the form of injectable solutions and help improve tissue trophism around the joints;
- B group vitamins - are shown to normalize the transmission of nerve impulses, which is especially important when nerves are compressed by defective bone structures.
For acute pain that cannot be eliminated with the help of tablets, intra-articular or periarticular block can be performed on the patient. They are carried out exclusively by qualified health workers in medical institutions and involve the introduction into the joint cavity or directly the area around it anesthetic solution with corticosteroids.
exercise therapy
Therapeutic exercise is an effective method of addressing decreases in muscle tone and mobility limitations. Thanks to a properly selected set of exercises, it is possible to increase the range of motion and reduce the severity of pain. They also prevent muscle atrophy and help relieve spasms if coxarthrosis is accompanied by pinching of nerve fibers, which reflexively leads to individual muscle spasms.
Exercise therapy classes can improve blood circulation in areas of degenerative-dystrophic processes. Due to this, the quality of trophism of diseased joints increases and the regenerative process is accelerated.
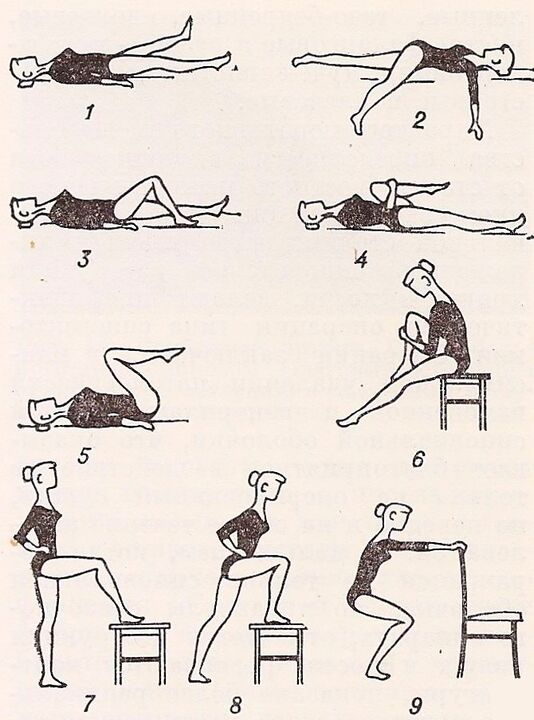
For each patient, a set of exercises should be developed individually by a specialist. At the same time, not only the degree of destruction of the hip joint is taken into account, but also the degree of physical development of the patient.
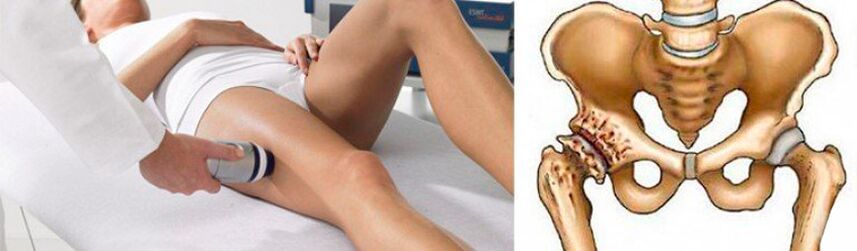
Physiotherapy
Physiotherapeutic procedures and massages have anti-inflammatory, analgesic, tonic, anti-edematous effects. In addition, it helps maintain normal leg muscle tone, preventing atonia and their atrophy.
With coxarthrosis of the hip joint, a course of 10-15 procedures is prescribed:
- ultrasound therapy;
- magnetotherapy;
- laser therapy;
- electrophoresis;
- ultrafonforesis;
- UHF;
- paraffin treatment.
Also, many patients are offered mud therapy. Such a procedure has a positive effect only in the first stage of development of coxarthrosis of the hip joint or during recovery after surgical treatment. Thanks to the therapeutic mud, it is possible to achieve an improvement in the quality of blood circulation and accelerate the recovery of motor ability of affected joints.
Plasmolifting
Plasmolifting or PRP-therapy is a procedure that involves the introduction of the patient’s own platelet-rich blood plasma into the hip joint cavity. This allows you to activate the hyaline cartilage recovery process.
But, according to some scientists, such a procedure can lead to the formation of malignant tumors. This view is based on the fact that plasmolifting promotes the formation of large numbers of stem cells, whose effects on the body have not been fully studied.
Surgical treatment of coxarthrosis of the hip joint
Despite significant discomfort in the hip joint, many are too late to seek medical help, when pathological changes in the joint reach 3 or even 4 degrees of severity, and its function is irreversible.
With advanced pathology, surgery is a necessary step. Only timely surgical intervention will help restore normal mobility and save the patient from excruciating pain, that is, to achieve a significant improvement in human quality of life. No drug, physiotherapeutic procedure, can restore severely destroyed cartilage. Best of all, painful intra-articular injections and medications can reduce pain. But this will be a temporary phenomenon, after which the pain will return again with equal or greater strength.
The indications for hip surgery are:
- loss of interarticular space;
- persistent pain in the hip joint, unacceptable;
- critical mobility disorders;
- broken hip.
Depending on the severity of the joint destruction and bone deformity, patients may be offered various types of surgical treatment, namely:
- arthrodesis;
- endoprosthesis;
- osteotomy.
Arthrodesis
Arthrodesis is an affordable operation that involves strong fixation of the articular bone with a metal plate. The result is complete immobilization of the joint. Therefore, with the help of arthrodesis, it is possible to correct only the support function of the foot, eliminating pain, but there is no need to talk about restoring mobility or a significant improvement in quality of life.
Today, arthrodesis is practically not used, as it prevents a person from the opportunity to move fully.
Endoprosthetics
Endoprosthetics with arthroplasty is the only way to radically solve the problem of coxarthrosis of the hip joint with the restoration of all its functions and motor abilities. This is a high-tech method of solving the problem of coxarthrosis, which allows you to completely forget about it for 15-30 years, as well as about the pain and restriction of mobility. Thanks to the use of modern endoprosthesis, it is possible to achieve full restoration of motor support function and provide patients with a normal life.
Surgery involves cutting off the femoral head and part of its neck. Surgical preparation of the acetabular bed was also performed, which involved removal of the osteophyte, alignment of its surface and resection of tissue that had undergone necrosis. Endoprosthetics can also be used to treat elderly patients with hip coxarthrosis.

The operation is performed under general anesthesia and takes about an hour. Depending on the severity of the degenerative-dystrophic process, surgery can be performed using one of the following methods:
- superficial - involves grinding the acetabulum and femoral head with further coating with a smooth implant that replaces the destroyed hyaline cartilage (this method is rarely used because of the possibility of inflammation of the periarticular tissues);
- unipolar - removal of the femoral head and its replacement with an endoprosthesis (used when cartilage is preserved on the surface of the acetabulum and only the femoral head is destroyed);
- bipolar - similar to the previous technique, only differing in the design of the endoprosthesis used, which has a lower coefficient of friction and provides smoother movement in the joint bed;
- total is the most effective and safest method of solving the problem of coxarthrosis of the hip joint, which involves complete resection of the femoral head with partial capture of its neck, as well as the acetabular fossa and replacing it with a complete prosthesis. articular joints.
Therefore, patients may be recommended to install various types of endoprosthesis. Most hip replacements are manufactured in the US and UK. For its manufacture, chemically and biologically inert metals are used: cobalt, chromium, titanium alloys. Often ceramics are also used. In most modern models, polymer pads are also used, which makes it possible to impart natural shock -absorbing, stabilizing and sliding properties to artificial TBS.
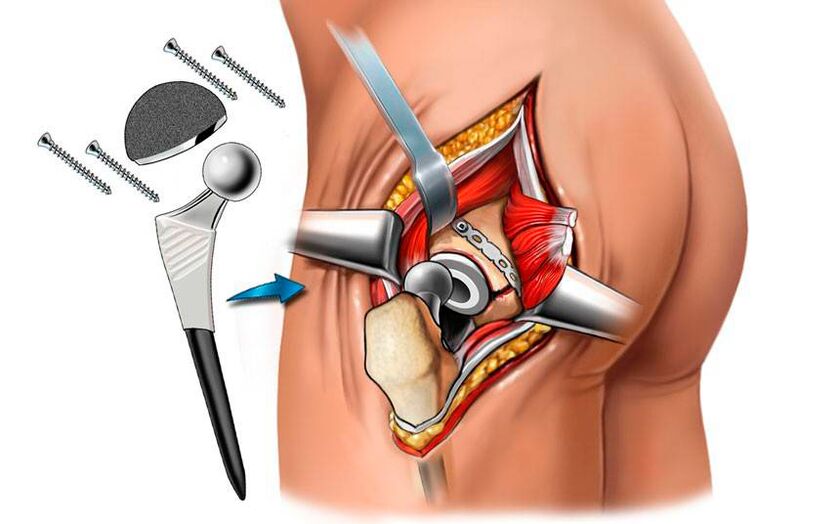
When performing endoprosthetics, the success of the operation is almost 100%.
After surgery, antibiotics were prescribed to prevent the development of infectious complications, and sutures were removed after 10 days. The size of the scar after surgery was approximately 8 cm At the same time, the patient was discharged from the clinic. Recovery after endoprosthetics is easy, but still requires physiotherapy, massage and exercise therapy.
osteotomy
Osteotomy is a surgical intervention that is a temporary step before the cardinal replacement of the hip joint with an artificial endoprosthesis. The essence of the operation is to align the axis of the femur due to intentional fracture. The resulting fragments are fixed in the most suitable position, thus slightly unloading the diseased joint. As a result, it is possible to temporarily reduce the severity of pain and increase mobility.
Thus, hip coxarthrosis is a rather formidable disease that can completely deny a person a chance to move freely. It develops for a long time, and its symptoms, especially in the early stages, are often considered by patients to be normal after doing physical exercise. But precisely in this case the dangerous disease lies, because only in the early stages of its development it can be treated by non -surgical means. But if the degenerative-dystrophic process has completely destroyed the hyaline cartilage and led to exposure of the bone surface, and even more so to flattening it, only surgery can help the patient. Fortunately, modern medical and surgical levels, in particular, make it possible to achieve complete restoration of the normal state of the hip joint and its function.
































